Colonoscopy Screening – Getting Started

Colonoscopy can stop colon cancer before it starts
Colorectal cancer has doubled in people under 50, but it’s easy to prevent. If you are 45 years or older,* it’s time to be your own health hero and start screening for colon cancer.
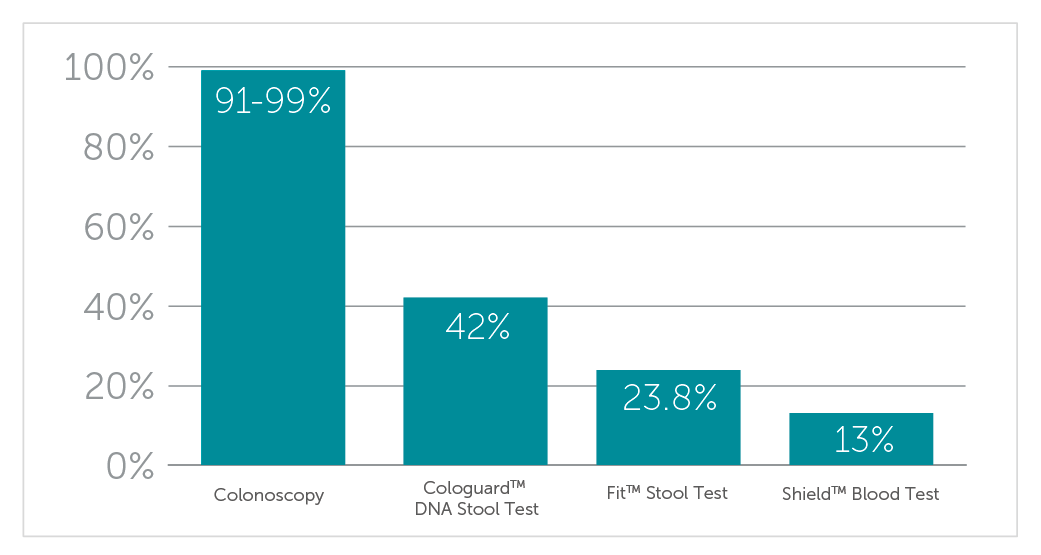
Colonoscopy is the gold standard for colon cancer screening
Colonoscopy is the only test that finds and removes polyps before they become cancer. Learn more about what to expect before, during, and after your colonoscopy screening here.
Don’t wait for peace of mind
Putting off screening could mean the difference between preventing colon cancer and a late-stage diagnosis. Click here to complete a brief pre-screening form. We can schedule most patients for a colonoscopy within 2-4 weeks without a pre-procedure office visit. A member of our GI team will review your information and contact you to schedule your colonoscopy or gather more information. Prefer to start with a phone call? Complete the first portion of the form and a team member will reach out to you.
* If you have a family history of colon cancer or other high-risk factors, talk to your doctor about screening earlier.