
Please note: In May 2021, the US Preventive Services Task Force updated its guidelines for colorectal cancer screening, lowering the recommended screening age from 50 to 45.
March is colon cancer awareness month, a great time to focus on reaching Americans eligible for screening. Colorectal cancer is the second leading cause of cancer death in the US.1 Fortunately, colorectal cancer can be prevented and the rate of colorectal cancer deaths in adults over age 50 has gone down over the last 20 years. This is mostly due to increased cancer screening, better cancer treatment, and Americans eating more healthy foods, exercising more, and smoking less.
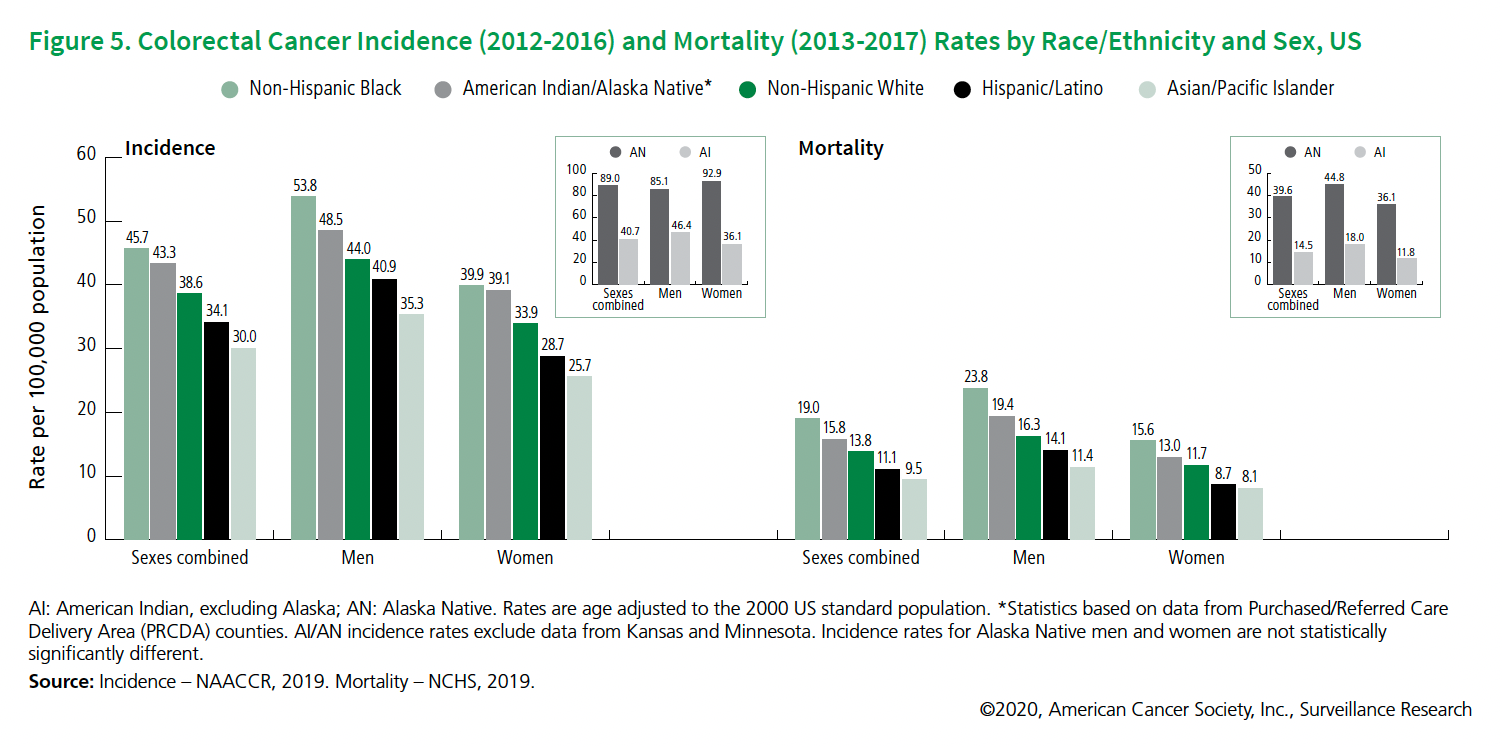 |
Colorectal cancer affects all population groups in the US, but because of various systemic and environmental inequities, African Americans are more affected by this cancer.1
- African Americans have the highest rates of colorectal cancer compared to all racial and ethnic groups in the US.
- African Americans are about 20% more likely to get colorectal cancer, and about 40% more likely to die from it than most other groups.
- African Americans are diagnosed with more advanced stage colorectal cancers and have the lowest five-year cancer survival rate of any racial group in the US.
- The highest colorectal survival rates are for Asian/Pacific Islanders (68%) and the lowest are for African Americans (60%).
- About half of the race-based differences in death from colon cancer are caused by less screening, differences in susceptibility, quality and timeliness of care, and lifestyle among African Americans.
What factors are contributing to these cancer disparities?2
- Lack of access to services and resources often creates barriers to getting health care. Examples include lower incomes and transportation issues, which limit the ability to find and access affordable healthcare. Those with lower incomes may have longer commutes to medical centers, lack transportation to medical sites, or live in communities with poor infrastructure.
- Geographic barriers to health care access. No matter their income level, Americans who live in rural communities or have mobility issues are also at risk of not getting or finding proper care.
- Difference in risk factor prevalence. Living environment can cause behaviors that increase the risk of cancer. People who live in neighborhoods that don’t have healthy food or safe areas for exercise are at risk for malnutrition and obesity, both of which have been linked to increased risk for colorectal cancer.
- Tumor biology factors and genetics may interact with factors such as diet, chronic stress, or tobacco exposure. Up to 30% of colorectal cancer patients have a family history of the disease.
- Systemic racism. There are many reasons for disparities in colon cancer screening and we have a growing awareness that many are rooted in systemic racism that influences the healthcare system just as it affects other institutions. Systemic racism is an important cause of inequities in the delivery of effective cancer prevention efforts.3
How can we help overcome barriers to colon cancer screening?
- Spread awareness and knowledge. Start thinking about screening for you or your family members. Don’t forget to ask your family about their health history.
- Increase accessibility to health care providers. Most doctor’s offices now have options for telehealth (online) virtual visits. Telehealth means you don’t have to drive to your visits and may reduce costs, making it easier to get the screenings you need.
- Explore screening options. Several good methods for colon cancer screening are available. Please talk with your primary care provider or gastroenterologist to find out which screening test is right for you.
- Support an equitable healthcare system. Medical systems, hospitals, communities, and the Centers for Disease Control and Prevention have declared racism a public health crisis and have developed plans to help make policies fairer and more equitable.
For more resources and information on disparities in health care
- https://www.ama-assn.org/delivering-care/patient-support-advocacy/reducing-disparities-health-care
- https://www.cancer.gov/about-nci/organization/crchd/about-health-disparities
References
1. American Cancer Society. Colorectal Cancer Facts & Figures 2020-2022. Atlanta: American Cancer Society; 2020.
2. National Cancer Institute (cancer.gov)
3. Barriers Driving Racial Disparities in Colorectal Cancer Screening in African Americans https://pubmed.ncbi.nlm.nih.gov/32647903/