Why take chances?
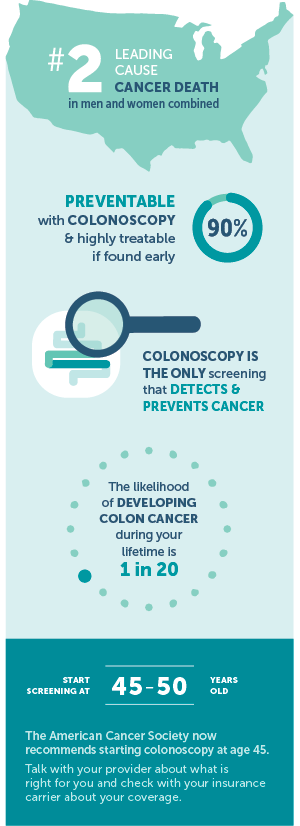
Colorectal cancer is the second most common cause of cancer-related death for men and women and about 5 percent of Americans will develop colorectal cancer in their lifetimes.1 The development of more than 75-90 percent of colorectal cancer can be avoided through early detection and removal of pre-cancerous polyps. Precancerous polyps can grow for years and transform into cancer without any symptoms. Colorectal polyps give rise to most colorectal cancer. As polyps accumulate mutations, high grade dysplasia can occur within the polyp. Given enough time, these dysplastic changes can become an invasive cancer.
RISK FACTORS FOR COLORECTAL CANCER
The US Preventive Task Force is looking to update their screening recommendation to begin at age 45 instead of age 50. If there is a family history of two or more first degree relatives with colorectal cancer/ advanced precancerous polyp or any first degree relative (parent, sibling, child) diagnosed under the age of 60, then we consider that as high-risk colon cancer screening. This increases the risk of colorectal cancer by 3-6 times compared to the general population and individuals with this high risk should begin screening at age 40 or 10 years before the age of the youngest relative with colorectal cancer.2
Inflammatory bowel disease such as Crohn’s colitis or Ulcerative Colitis increases the risk of colon cancer. Patients with these diagnoses should start screening 8 years after their colitis diagnosis.3
95 percent of colorectal cancers are sporadic, but about 5 percent of colorectal cancers are secondary to inherited gene mutations that cause syndromes such as familial adenomatous polyposis or hereditary non-polyposis colorectal cancer (Lynch syndrome). When patients are found to have a multitude of polyps or strong family histories of other cancers, this may prompt a genetic counselor referral to look for such gene mutations.
Importantly, lifestyle factors have also been found to increase the risk of colorectal cancer, including obesity, a diet low in fruit and vegetables, a high-fat diet, a diet high in processed meats, alcohol consumption, and tobacco use.
PREVENTION TESTS ARE BETTER THAN DETECTION TESTS
Colonoscopy is the preferred colorectal cancer prevention test because it has the highest sensitivity for colorectal cancer and precancerous polyps can be detected and removed in one procedure.
Alternatively, detection tests such as an annual fecal immunochemical test (FIT) can performed. However, if this is positive, prompt colonoscopy follow-up is necessary. FIT has similar detection rates of colorectal cancer compared to colonoscopy, but lower detection rates of advanced adenomas and precancerous polyps. Multi-target stool DNA testing, Cologuard, which combines fecal markers for hemoglobin and DNA mutation and methylation can be done every 3 years, and though has a higher sensitivity and specificity than FIT for colorectal cancer, it will miss more than 30 percent of polyps with advanced dysplasia. Similarly, if positive, prompt colonoscopy follow-up is necessary.4